More than four decades have passed since Estelle v. Gamble, the 1976 U.S. Supreme Court ruling that held prisoners cannot be denied necessary medical care under the Eighth Amendment. But when cash-strapped state Departments of Corrections charge co-pays for healthcare provided to sick prisoners – who earn meager wages and are the least able to afford such fees – the effect can often be the same.
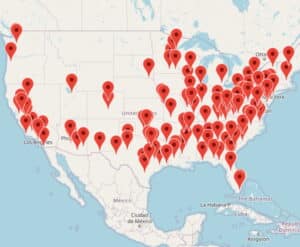
According to the Brennan Center for Justice, at least 38 states charge prisoners a co-pay for medical services. Another four allow such fees to be charged by local jails. The co-pays range from $2.00 per nurse or doctor visit to a one-time $100 annual charge. Federal prisoners are also subject to fees for medical care, and charging co-pays has been a longstanding practice in prison systems. [See: PLN, Jan. 1996, p.8].
Officially, the fees are meant to reimburse corrections agencies for the cost of providing medical services. However, they don’t come close to doing so. The Pew Charitable Trusts reported that Pennsylvania, which charges prisoners a $5.00 co-pay, collected just $373,000 of the $248 million spent on prison health care in 2014 – less than two-tenths of one percent. Michigan collected $200,000 of the $300 million it paid that year. In comparison, California collected approximately $500,000 of the $2.2 billion state prison officials spent on medical care – both less than one-tenth of one percent.
Oklahoma’s $4.00 co-pay is just over the national average of $3.47. In 2016, the Oklahoma Department of Corrections (DOC) collected $250,000 from prisoners – a “very small portion” of the $84.4 million it spent on health care that year, acknowledged DOC spokesman Mark Myers.
But while the co-pays are a drop in the bucket of prison expenses, the cost they represent to prisoners and their families is high. An April 2017 study by the Prison Policy Initiative (PPI) compared prisoners’ hourly pay to the minimum wage earned by non-prisoners to devise a co-pay adjusted for prison earnings. PPI determined that 14 states collect a co-pay equivalent to charging more than $200 to employees who earn the minimum wage outside prison – over two-thirds of the $290 those workers earn in a 40-hour work week.
In West Virginia, where prisoners make as little as 4 cents per hour, the DOC’s $5.00 co-pay is equivalent to one that costs $1,093.75 for minimum wage workers on the outside – almost an entire month’s paycheck. Even in a state like California, where the pay is higher both in and outside of prison, the $5.00 co-pay imposed on prisoners is equivalent to $656.25 for minimum-wage earners in the free world.
Alabama, Georgia, Florida, and Texas lack any guaranteed wages for prison labor – meaning it’s possible that a prisoner can never earn enough to cover the cost of a medical co-pay in those states. While those who can’t afford to pay are not denied health care, the amount owed is deducted from any money they receive or earn in the future.
Prison officials acknowledge that co-pays deter prisoners from seeking medical care but insist the fees are needed to – as Myers put it – prevent “frivolous use of the medical system.”
“We do it for the same reason your insurance company does – to eliminate abuse by making the inmates put a little skin in the game,” said Tommy Thompson, a local jail administrator in Tennessee.
In Nevada, which charges one of the highest prisoner co-pays in the United States, DOC Public Information Officer Brooke Keast justified the $8.00-per-visit fee by saying prisoners tend “to be people who have not put their health as a priority,” so it is “a constant guess as to whether they are really hurting.”
“Correctional people may think it’s a deterrent for this annoying population who just wants attention,” said Wendy Sawyer, a policy analyst with PPI, “but in reality, they probably have a lot of legitimate health concerns to be addressed.”
Co-pays are charged to a prisoner’s trust account, which is funded from two primary sources – prison wages and money received from family and friends. The accounts also pay for commissary items like hygiene products, food, postage stamps, and clothing.
As a practical matter, the use of co-pays sets up a “two-tier” prison medical system, according to the National Commission on Correctional Health Care (NCCHC) – one for prisoners who can afford both medical care and commissary purchases such as deodorant, another for those forced to choose between the two. NCCHC opposes co-pays for medical treatment.
While corrections officials are prohibited from denying care when prisoners cannot pay, they can seize up to half the funds in a prisoner’s trust account to cover outstanding co-pay costs, and negative balances can follow them even after their release. In Texas, where Estelle v. Gamble originated, Kyle Walker said she “can only afford to spend $30 to $40 every couple of weeks” to send to her imprisoned boyfriend.
“Even to just put the money in his trust fund, there’s a fee for that transaction,” she said. “So for them to deduct half of the money for [medical] services he’s already received – it defeats the purpose of me even sending him money.”
Faced with this harsh calculation, prisoners sometimes delay or decline to seek medical care – thereby not only risking their health but also the health of others if they contract contagious diseases while causing their medical costs to balloon if their untreated condition later worsens. Those costs often fall on the state anyway – either when prisoners are still incarcerated or after their release, when they receive medical care in the community through Medicaid or emergency room visits.
“The health of the prison population is worse on average – if not much worse – than the general public, so to have this [co-pays] in place in any prison is unethical,” said J. Wesley Boyd.
Boyd, an associate professor of psychiatry at Harvard University, is a member of the school’s Center for Bioethics who co-wrote a 2009 study that found widespread shortcomings in prison medical systems.
Health care is “one of the few areas where correctional facilities have control over [their] budget,” said Brad Brockmann, executive director for the nonprofit Center for Prisoner Health and Human Rights. “Somebody who doesn’t come in [for medical care] is somebody who isn’t costing them anything,” he added.
Robert Greifinger, former chief medical officer for the New York State Department of Corrections and Community Supervision, agreed that “there are ways to deal with the high demand [for health care] other than co-pays,” which he called “punitive.”
Jerry Madden is the former state representative who came up with the law that created a $100 annual medical co-pay for prisoners in Texas. He said they would have just “a couple less candy bars they could buy from the commissary,” even though most Texas prisoners receive no pay for their prison work assignments. [See: PLN, Feb. 2015, p.18; Oct. 2012, p.42].
Sawyer, with the Prison Policy Initiative, called co-pays imposed on prisoners “another way of nickel and diming people who don’t have anything.”
NCCHC insists that “a good triage system” to manage potential abuse of sick calls is preferable to the harm that co-pays pose for the health of prisoners and prison staff, as well as the general public, with which both eventually interact.
“Charging prisoners for health care is yet another way of kicking them when they’re down,” concluded Dr. Josiah Rich, a professor of medicine at Brown University who directs a clinic in a Rhode Island prison.
Legal challenges to medical co-pays in prisons and jails have been upheld by many courts, including in Poole v. Isaacs, 703 F.3d 1024 (7th Cir. 2012). However, over 25 years ago, the Tenth Circuit Court of Appeals upheld a challenge to a co-pay statute in Colorado, which was amended due to the litigation. See: Collins v. Romer, 962 F.2d 1508 (10th Cir. 1992).
Sources: www.prisonpolicy.org, www.vice.com, www.pewtrusts.org, www.npr.org, www.huffingtonpost.com, www.readfrontier.org
Originally published in Prison Legal News on January 31, 2018.
Published Feb 1, 2018 by Christopher Zoukis, JD, MBA | Last Updated by Christopher Zoukis, JD, MBA on Feb 20, 2024 at 9:29 pm